- Iron National Institute of Health, Office of Dietary Supplements
- Iron Linus Pauling Institute
- List of foods high in iron US Department of Agriculture
- Iron WebMD
- Love AL et al, 2008, Obesity, bariatric surgery, and iron deficiency: true, true, true and related PubMed
- Fernández-Bañares F et al, 2009, A short review of malabsorption and anemia PubMed Central
- Beyan C et al, 2007, Post-gastrectomy anemia: evaluation of 72 cases with post-gastrectomy anemia PubMed
- Sachdev AH et al, 2013, Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance PubMed Central
- Burger SE et al, 2002, How to asses iron deficiency anemia and use the hemocue? USAID
- Hurrel L et al, 2010, Iron bioavailability and dietary reference values The American Journal of Clinical Nutrition
- Hallberg L et al, 1993, Inhibition of haem-iron absorption in man by calcium PubMed
- Hunt JR, 2006, Bioavailability of iron, zinc and copper as influenced by host and dietary factors US Department of Agriculture
- Nestel P, 1995, Iron interventions for child survival USAID
- Powers HJ, 2003, Riboflavin (vitamin B-2) and health The American Journal of Clinical Nutrition
- Gordeuk VR et al, 1987, High-dose carbonyl iron for iron deficiency anemia: a randomized double-blind trial The American Journal of Clinical Nutrition
- Restless legs syndrome and related disorders University of Maryland
- Thankacan P et al, 2008, Iron absorption in young Indian women: the interaction of iron status with the influence of tea and ascorbic acid The American Journal of Clinical Nutrition
- Ma Q et al, Bioactive Dietary Polyphenols Inhibit Heme Iron Absorption in A Dose-Dependent Manner in Human Intestinal Caco-2 cells PubMed Central
- Mascitelli L et al, 2010, Inhibition of iron absorption by polyphenols as an anti-cancer mechanism QJM
- Ballot D et al, 1987, The effects of fruit juices and fruits on the absorption of iron from a rice meal PubMed
- Cook JD et al, 2001, Effect of ascorbic acid intake on nonheme-iron absorption from a complete diet The American Journal of Clinical Nutrition
- Hunt JR et al, 1994, Effect of ascorbic acid on apparent iron absorption by women with low iron stores US Department of Agriculture
- Fidler MC et al, 20014, Erythorbic acid is a potent enhancer of nonheme-iron absorption The American Journal of Clinical Nutrition
- Monsen ER et al, 1976, Food iron absorption in human subjects lv. The effects of calcium and phosphate salts on the absorption of nonheme iron The American Journal of Clinical Nutrition
- Jacobs P et al, 1964, Role of hydrochloric acid in iron absorption Journal of Applied Physiology
- Hallberg L et al, 1982, Effect of different drinks on the absorption of non-heme iron from composite meals PubMed
- Zimmermann MB et al, 2008, Adiposity in women and children from transition countries predicts decreased iron absorption, iron deficiency and a reduced response to iron fortification PubMed
- Charlton RW et al, 1964, Effect of Alcohol on Iron Absorption PubMed Central
- Turgut S et al, 2007, Interaction between anemia and blood levels of iron, zinc, copper, cadmium and lead in children PubMed
- Hoolbrook JT et al, Dietary fructose or starch: effects on copper, zinc, iron, manganese, calcium, and magnesium balances in humans The American Journal of Clinical Nutrition
- Fox MR et al, 1980, Effects of vitamin C and iron and cadmium metabolism PubMed
- Ziegler EE, 2007, Adverse effects of cow’s milk in infants PubMed
- EFSA Panel on Food Additives and Nutrient Sources added to Food (ANS), 2010, Scientific Opinion on the safety of heme iron (blood peptonates) for the proposed uses as a source of iron added for nutritional purposes to foods for the general population, including food supplements European Food Safety Authority
- Hershko C et al, 2007, A hematologist’s view of unexplained iron deficiency anemia in males: impact of Helicobacter pylori eradication PubMed
- Annibale B et al, 2003, Concomitant alterations in intragastric pH and ascorbic acid concentration in patients withHelicobacter pylori gastritis and associated iron deficiency anaemia BMJ
- Hurrel RF et al, 1999, Inhibition of non-haem iron absorption in man by polyphenolic-containing beverages PubMed
- Tuntipopipat S et al, 2006, Chili, but Not Turmeric, Inhibits Iron Absorption in Young Women from an Iron-Fortified Composite Meal The Journal of Nutrition
- Tuntawiroon M et al, 1991, Dose-dependent inhibitory effect of phenolic compounds in foods on nonheme-iron absorption in men The American Journal of Clinical Nutrition
- Fei C, 2015, Iron Deficiency Anemia: A Guide to Oral Iron Supplements Clinical Correlations
- Comparison of oral iron supplements, 2008 (from Pharmacist’s Letter) Thezlifemag.com
- Cook JD et al, 1991, Calcium supplementation: effect on iron absorption The American Journal of Clinical Nutrition
- Sharma VR et al, 2004, Effect of omeprazole on oral iron replacement in patients with iron deficiency anemia PubMed
- Committee on Nutrition, 1992, The Use of Whole Cow’s Milk in Infancy Pediatrics
- Skikne BS et al, 1981, Role of gastric acid in food iron absorption PubMed
- Sotelo A et al, 2010, Role of oxate, phytate, tannins and cooking on iron bioavailability from foods commonly consumed in Mexico PubMed
- Disler PB et al, 1975, The effect of tea on iron absorption PubMed
- 2011, GRAS Notification for Phytic Acid (50% Solution) US Food and Drug Administration
- Milman N et al, 2014, Ferrous bisglycinate 25 mg iron is as effective as ferrous sulfate 50 mg iron in the prophylaxis of iron deficiency and anemia during pregnancy in a randomized trial PubMed
Iron
What is iron?
Iron is a mineral that is an essential nutrient to human life and health.
The chemical symbol for iron is Fe.
Iron Functions
- Iron, as part of hemoglobin, carries oxygen in the blood, and as part of myoglobin in muscles, it carries oxygen in the muscles.
- As part of certain enzymes iron is involved in the metabolism and immunity.
How much iron do you need per day?
The Recommended Dietary Allowance (RDA) for iron for healthy people with normal blood iron levels [1]:
Chart 1. RDA for Iron |
|
| Age | Iron (mg/day) |
| 0-6 months | Breast milk or formula* |
| 7-12 months | 11 |
| 1-3 years | 7 |
| 4-8 years | 10 |
| 9-13 years | 8 |
| 14-18 years boys | 11 |
| 14-18 years, girls | 15 (26 for vegans) |
| 19+, men | 8 (14 for vegans) |
| 19+, menstruating women | 18 (33 for vegans) |
| Pregnant women | 27 |
| Breastfeeding women | 10 |
| Women after menopause | 8 (14 for vegans) |
Chart 1 source: NIH.gov, Office of Dietary Supplements [1]. NOTE: Cow’s milk is low in iron and it can cause gastrointestinal bleeding, so it should not be given to infants before 1 year of age [32,43]. Individuals regularly engaging in hard exercise may need 30% more iron than the RDA listed above [1].
Heme and Nonheme Iron
Dietary iron can appear as:
- Nonheme iron in plant foods, milk products, eggs and iron-fortified foods
- Heme iron in meat and fish; heme iron comes from the hemoglobin in the blood and myoglobin in the muscles.
Heme iron is about 1.8 times as bioavailable as nonheme iron, which means you need to get about twice as much iron from plant foods than from animal foods to get the same effect [1].
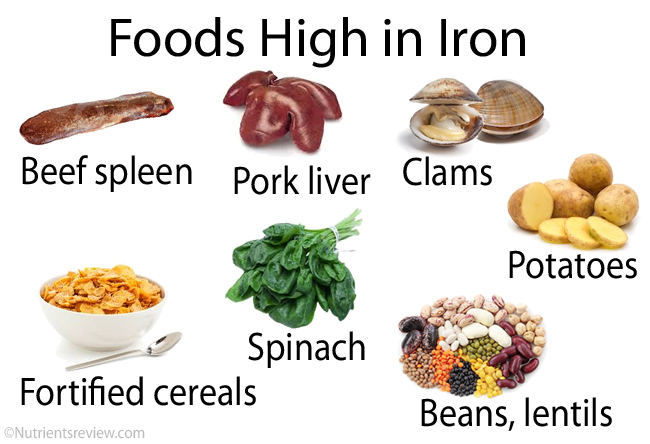
Picture 1. Foods rich in iron
Chart 2. List of Foods High in Iron |
|
ANIMAL FOODS (heme iron) |
Iron (mg) |
| Beef or lamb spleen (3 oz, 85 g) | 33 |
| Pork spleen (3 oz, 85 g) | 19 |
| Pork liver (3 oz, 85 g) | 15 |
| Clams (3 oz, 85 g) | 12 |
| Chicken giblets (liver, heart, kidneys) (3 oz, 85 g) | 5-9 |
| Cuttlefish, mussels, octopus, oysters, whelks (3 oz, 85 g) | 2-9 |
| Beef liver (3 oz, 85 g) | 6 |
| Beef (3 oz, 85 g) | 2-5 |
| Bison, deer, horse, moose (3 oz, 85 g) | 4 |
| Sardines and anchovies (European) with bones (3 oz, 85 g) | 4 |
| Goat (3 oz, 85 g) | 3 |
| Shrimps, canned (3 oz, 85 g) | 2 |
| Chicken, duck, turkey (3 oz, 85 g) | 1-2 |
| Fish: bass, catfish, haddock, halibut, herring, mackerel, trout, tuna (3 oz, 85 g) | 1 |
PLANT FOODS (nonheme iron) |
|
| Cereals ready-to-eat, fortified (30 mg dry = 1 cup, prepared) | 6-18 |
| Oats, instant, prepared (1 cup, 237 mL) | 6 |
| Amaranth, teff (1 cup, 237 mL) | 5 |
| Soybeans (1/2 cup, 120 mL) | 4.5 |
| Legumes: beans, chickpeas, lentils (1/2 cup, 120 mL) | 2-5 |
| Pumpkin seeds (1 oz, 28 g) | 4 |
| Blackstrap molasses (1 tbsp, 20 g) | 3.5 |
| Bagel, biscuit (4″ dia) | 3.5 |
| Spinach, boiled (1/2 cup, 120 mL) | 3 |
| Grains: quinoa, rice, spelt, wheat kamut (1 cup, 237 mL) | 3 |
| Prune juice (1 cup, 237 mL) | 3 |
| Beets, canned (1/2 cup, 120 mL) | 3 |
| Cornflakes (1 oz dried = 1 cup prepared ) | 2.5 |
| Tofu (2 oz, 57 g) | 2.5 |
| Potatoes, sweet potatoes (1 cup, 237 mL) | 2 |
| Grains: barley, bulgur (1 cup, 237 mL) | 2 |
| Figs, dried (2 oz, 57 g) | 2 |
| Sunflower seeds (1 oz, 28 g) | 2 |
| Cashew nuts (1 oz, 28 g) | 2 |
| Bread, white or whole-wheat (2 slices, 50 g) | 2 |
| Cabbage (Chinese) (1 cup, 237 mL) | 2 |
| Swiss chard, cooked (1/2 cup, 120 mL) | 2 |
| Bulgur (1 cup, 237 mL) | 2 |
| Strawberries (1 cup, 237 mL) | 1.5 |
Chart 1 sources: USDA.gov [3] All listed foods are ready to eat.
Human breast milk contains about 0.3 mg iron/liter. About 50% of iron from breast milk is absorbed [1]. Breast milk is a sufficient source of iron for healthy infants up to their 6 months of age. The Adequate Intake (AI) for iron for 0-6 months old infants is 0.27 mg/day and for 7-12 months old infants 11 mg/day [1].
Iron Deficiency: Causes, Symptoms
Iron deficiency may, in few months after stopping iron intake, result in iron deficiency anemia.
Symptoms may include paleness, bluish eye whites, fatigue, dizziness, rapid heart beat, rapid breathing even during moderate exertion, feeling cold, brittle nails, inflamed tongue, mouth sores, restless leg syndrome, eating dirt or other non-nutrient substances (the disorder is called ‘pica’) [1].
Causes [1]:
- Insufficient iron intake due to vegetarian diet (especially in women and athletes), chronic alcoholism, anorexia nervosa, starvation, red meat intolerance after bariatric surgery [5]
- Low iron absorption can be due to small intestinal disorders, such as celiac disease [6], Crohn’s disease, intestinal parasites, stomach infection by the bacterium Helicobacter pylori associated with achlorhydria [6], vitamin C deficiency or due to partial gastric resection [6,7] or gastric bypass (bariatric surgery) in treatment of obesity [6] or, rarely, small intestinal bacterial overgrowth (SIBO) [8].
- Excessive iron loss due to chronic bleeding from the gastrointestinal tract (in peptic ulcer, nonsteroidal anti-inflammatory drugs, such as aspirin or ibuprofen, alcoholism, intestinal worms) [9], colorectal cancer, chemotherapy), intrauterine device and other causes of heavy menstruation
- Individuals who have hemolytic anemia due to malaria or sickle cell disease [9]
- Chronic kidney disease due to low synthesis of erythropoetin, which is needed for synthesis of hemoglobin, or due to kidney dialysis during which iron is lost from the blood
- Low iron bioavailability due to copper, vitamin A [10] or vitamin B2 (riboflavin) deficiency [10], inflammatory diseases, such as rheumatoid arthritis, or cancer.
Who else is at risk to develop iron deficiency anemia: [1,2]
- Preterm and low-weight infants due to low iron stores
- Infants fed with cow’s milk, which is low in iron
- Children between 6 months and 4 years, because they have low iron stores and increased needs due to fast growth
- Teenage girls due to fast growth and menstruation
- Pregnant and breastfeeding women
- Women athletes, vegetarian athletes, high distance runners, possibly due to increased microscopic bleeding in the gastrointestinal tract and feet
- People who frequently donate blood
People at risk for developing iron deficiency should try to eat sufficient amount of iron-rich foods. For pregnant women with confirmed iron deficiency, the U.S. Center for Disease Control and Prevention (CDC) recommends at least 30 mg iron per day [1].
Diagnosis of Iron-Deficiency Anemia
A doctor can give a diagnosis of iron deficiency anemia after the following blood tests results:
- Low MCV [mean corpuscular volume], which means small erythrocytes, and low MCHC [mean corpuscular hemoglobin concentration], which means lowered concentration of hemoglobin in erythrocytes, from which a term microcytic hypochromic anemia originates.
- Low HCT (HCT or hematocrit is red blood cells volume/blood volume ratio)
- Low iron
- Low hemoglobin
- Low ferritin
- High TIBC [total iron binding capacity], meaning that due to iron deficiency transferrin has more room to bind iron
When bleeding in the gastrointestinal tract is suspected as a possible cause of anemia, a stool test for blood should be done, and, if positive, an upper endoscopy or colonoscopy to find the exact site of bleeding may be done.
Iron Supplements
Oral Supplements
Without prescription (over-the-counter):
- Some multivitamin/mineral supplements contain some iron (typically 18 mg), which is Recommended Dietary Allowance for menstruating women, but is not sufficient to treat iron deficiency anemia. Before using iron supplements, speak with your doctor about the appropriate dose and form. Do not take iron supplements without doctor’s approval, if you are pregnant, have a liver or other disease, you are allergic to anything or you take other drugs or supplements.
Chart 3. Iron Supplements |
||
| FORM | BIOAVAILABILITY | SIDE EFFECTS |
| Heme-iron polypeptides [33,40] | Good | Less |
| Ferrous ascorbate (iron + vitamin C) [39] | Good | |
| Carbonyl iron [15,40] | Slowly absorbed but good bioavailability | Less |
| Iron salts: ferrous fumarate, gluconate, lactate and sulfate | Moderate | Usual |
| Iron chelates with organic acids: ferrous aspartate, bisglycinate [40,48] and succinate | Moderate | Less |
| Polysaccharide-iron complexes [39,40] | Moderate | Unknown |
| Ferric ammonium citrate [40] | Poor | Less |
| Enteric coated or controlled release iron [39] | Poor | Less |
NOTE: Heme iron supplements are more bioavailable than nonheme ones and ferrous forms more than ferric ones. Oral iron supplements are available as tablets, chewables, capsules, suspensions or solutions.
You should take iron supplements with water on an empty stomach at least 30 minutes before meals. You can take iron with a small amount of food to prevent stomach irritation. Food can decrease the absorption of iron by up to 50% [40].
Injections
Intravenous or intramuscular injections are intended mainly for individuals with iron deficiency who can not tolerate oral supplements.
- Iron dextran and ferumoxytol may be given in a single large dose.
- Ferric gluconate and iron sucrose are given in smaller doses.
Side effects of iron injections may include flushing, headache, dizziness, rashes, fever, pain at the injection site, and, rarely, anaphylactic shock, which may be fatal (mainly after iron dextran or ferumoxytol).
The effectiveness of iron supplements in treating iron-deficiency anemia is confirmed by increasing levels of reticulocytes (immature erythrocytes, reflecting increased erythrocyte production) in the blood few days after starting treatment and later, by increasing hemoglobin levels.
Iron Supplements Benefits
Iron supplements are EFFECTIVE for [1]:
- Prevention or treatment of iron deficiency
- Treating anemia caused by chronic heart, kidney, gastrointestinal disease, cancer
Iron supplements are POSSIBLY EFFECTIVE for prevention or treatment of certain conditions in individuals with iron deficiency (but not in those with normal blood iron levels) [2,4]:
- Learning problems in children
- Preventing lead intoxication
- Coughs caused by ACE inhibitors (captopril, enalapril, lisinopril)
- Symptoms of heart failure
- Restless leg syndrome (RLS) [16].
There is INSUFFICIENT EVIDENCE about the effectiveness of iron supplements in attention deficit-hyperactivity disorder (ADHD), depression, fatigue in people with normal iron levels, improving athletic performance, canker sores, Crohn’s disease, female infertility, heavy menstrual bleeding [1,4].
Who should NOT take iron supplements?
Adult men and women after menopause with normal blood iron levels and individuals with hemochromatosis, sideroblastic or hemolytic anemia should not take iron supplements without a doctor’s approval in order to avoid iron overload [1,2].
Iron Supplements Safety: Side Effects, Toxicity
The human body cannot get rid of excess iron quickly (only small amounts are lost in the urine and sweat), so taking iron supplements in absence of iron deficiency increases the risk of iron toxicity. The Tolerable Upper Intake Level (UL)–the dose that should not be toxic–for iron, is 40 mg/day before 14 years of age and 45 mg/day after 14 years of age [1].
Side effects of prescribed doses of oral iron supplements may include nausea, vomiting, abdominal cramps, constipation, diarrhea, temporary staining of the teeth (especially with liquid iron supplements) and black or green stool [1].
Iron supplements may worsen stomach ulcers or intestinal ulcers in ulcerative colitis or Crohn’s disease and may increase the risk of malaria and pneumonia in children in tropical areas [1,2]. To avoid or reduce iron side effects, you may initially take a half of the dose, followed by the full dose after few days, or get iron by intravenous injections. Eventual harmful effects of iron supplements taken by a mother for the unborn baby are neither confirmed, nor excluded.
Allergic reaction, mainly to iron dextran injections, may include metallic taste in the mouth, facial swelling, drop of blood pressure, or death.
Iron overdose (acute iron poisoning) my occur after ingesting 20-60 mg of iron/kg body weight. 200 mg iron taken at once can be deadly for a child. Symptoms of overdose appear within 1-6 hours of ingestion and include nausea, vomiting, abdominal pain, tarry stools, lethargy, weak and rapid pulse, low blood pressure, fever, difficulty breathing, coma and, often, death; if a victim survives, symptoms may subside for 12 to 48 hours after the iron ingestion and may include heart, kidney, liver, blood or brain damage, of which some may be permanent.
Iron overload (chronic iron poisoning) is a condition, in which, despite a normal iron intake, excess iron builds up in the internal organs and causes cirrhosis of the liver, diabetes, heart muscle damage, or joint problems. This may happen in hereditary hemochromatosis or after repeated transfusions (in sideroblastic anemia, thalassemia major). Rarely, iron overload may occur in individuals with normal blood iron levels taking high doses of iron supplements. To avoid iron overload, iron supplements should never be taken without an obvious reason – iron deficiency or a risk of developing it.
Iron Absorption, Body Stores, Interaction With Foods and Drugs
About 15-35% of heme iron from meat and fish and 2-20% of non-heme iron from plant foods, eggs and dairy products are absorbed in the small intestine–mostly in the duodenum–and, to a smaller extent, in the colon [1,10].
Factors that INCREASE the absorption of the nonheme iron from plant foods, milk, eggs and fortified foods:
- Meat, poultry and fish [1,2,9,10]
- Vitamin C from supplements, fortified foods [17], or fruits/juices high in vitamin C: lemon, orange or apple juice, guava, pineapple or pawpaw (Carica papaya) [9,13,20,21,22]
- Erythorbic (isoascorbic) acid, a vitamin C derivative, commonly added to processed meats, baked goods, jams and vegetable juices [13]
- Supplemental hydrochloric acid [13] (in individuals with low gastric acid)
- Low body iron (ferritin) stores [10,12]
- Pregnancy [13]
- Whisky, brandy, beer, red and white wine; alcoholics often have abnormally increased iron stores (hemochromatosis) [9,13,28].
Factors that DECREASE the absorption of the nonheme iron from plant foods, milk, eggs and fortified foods:
- Absent or low gastric acid (achlorhydria or hypochlorhydria) due to chronic gastritis caused by Helicobacter pylori infection [34,35] or autoimmune atrophic gastritis in pernicious anemia
- Tannins and polyphenols in cocoa [36], black and green tea [9,13,19,46], herbal teas (peppermint, chamomile, vervain, lime flower) [36], coffee [9,26], sorghum [13], chili [37], oregano [9,13], chocolate and Yod Kratin (a vegetable in South Asia) [38]
- Phytates in bran (wheat, oats, barley), wheat germ, whole grains, seeds, walnuts, sweet almonds, beans (except green beans), peas, lentils, soy, rolled oats, rice [1,2,9,12,45]. According to some long-term studies, phytates did not decrease the bioavailability of iron, though [47].
- Soy protein and proteins in milk, whey and egg whites (casein, albumin) [9,10,12,13]
- Maize (cornmeal, tortilla) [9]
- Recent iron intake [13]
- Calcium from dairy products [4,18,24] but less likely from supplements [11,13,41]
- Zinc supplements taken with water but not with meal [12]
- Drugs that lower stomach acidity (antacids, such as calcium carbonate, H2 blockers, such as ranitidine and cimetidine [44], proton pump inhibitors ( omeprazole [42]), cholestyramine (cholesterol-lowering resin), levodopa, levothyroxine, methyldopa, penicillamine, quinolones, tetracyclines, and bisphosphonates [1]
- Cadmium [31], lead [29], cobalt [13], strontium, manganese [13], copper [13,29]
- Vitamin A (retinol) and vitamin B2 (riboflavin) deficiency [10]
- Obesity [10,27]
- Hemochromatosis, alpha-thalassemia 1 and beta-talasssemia [10]
Once in the blood, iron binds to a protein transferrin and becomes available for the incorporation into hemoglobin in the red blood cells whenever needed. Iron in excess of immediate needs is stored as ferritin (an iron-protein compound) in the liver, spleen and bone marrow.
Allopurinol (for treatment of gout), may increase the iron storage in the liver, so it should not be used in combination with iron supplements [1].
Iron supplements (but not iron from foods) may decrease the absorption and thus reduce effectiveness of zinc, certain antibiotics (such as ciprofloxacin, demeclocycline, minocycline, tetracycline), or other drugs, such as bisphosphonates (alendronate, etidronate), levodopa, methyldopa, levothyroxine, mycophenolate mofetil and penicillamine [4].
Therefore, it is recommended to take iron supplements at least two hours apart from abovementioned foods and drugs.
Minerals
- Fructose
- Galactose
- Glucose
- Isomaltose
- Isomaltulose
- Lactose
- Maltose
- Mannose
- Sucrose
- Tagatose
- Trehalose
- Trehalulose
- Xylose
- Erythritol
- Glycerol
- Hydrogenated starch hydrolysates (HSH)
- Inositol
- Isomalt
- Lactitol
- Maltitol
- Mannitol
- Sorbitol
- Xylitol
- Fructo-oligosaccharides (FOS)
- Galacto-oligosaccharides (GOS)
- Human milk oligosaccharides (HMO)
- Isomalto-oligosaccharides (IMO)
- Maltotriose
- Mannan oligosaccharides (MOS)
- Raffinose, stachyose, verbascose
- SOLUBLE FIBER:
- Acacia (arabic) gum
- Agar-agar
- Algin-alginate
- Arabynoxylan
- Beta-glucan
- Beta mannan
- Carageenan gum
- Carob or locust bean gum
- Fenugreek gum
- Galactomannans
- Gellan gum
- Glucomannan or konjac gum
- Guar gum
- Hemicellulose
- Inulin
- Karaya gum
- Pectin
- Polydextrose
- Psyllium husk mucilage
- Resistant starches
- Tara gum
- Tragacanth gum
- Xanthan gum
- INSOLUBLE FIBER:
- Cellulose
- Chitin and chitosan
- FATTY ACIDS
- Saturated
- Monounsaturated
- Polyunsaturated
- Short-chain fatty acids (SCFAs)
- Medium-chain fatty acids (MCFAs)
- Long-chain fatty acids (LCFAs)
- Very long-chain fatty acids (VLCFAs)
- Monoglycerides
- Diglycerides
- Triglycerides
- Vitamin A - Retinol and retinal
- Vitamin B1 - Thiamine
- Vitamin B2 - Riboflavin
- Vitamin B3 - Niacin
- Vitamin B5 - Pantothenic acid
- Vitamin B6 - Pyridoxine
- Vitamin B7 - Biotin
- Vitamin B9 - Folic acid
- Vitamin B12 - Cobalamin
- Choline
- Vitamin C - Ascorbic acid
- Vitamin D - Ergocalciferol and cholecalciferol
- Vitamin E - Tocopherol
- Vitamin K - Phylloquinone
- Curcumin
- FLAVONOIDS:
- Anthocyanidins
- Flavanols: Proanthocyanidins
- Flavanones: Hesperidin
- Flavonols: Quercetin
- Flavones: Diosmin, Luteolin
- Isoflavones: daidzein, genistein
- Caffeic acid
- Chlorogenic acid
- Lignans
- Resveratrol
- Tannins
- Tannic acid
- Alcohol chemical and physical properties
- Alcoholic beverages types (beer, wine, spirits)
- Denatured alcohol
- Alcohol absorption, metabolism, elimination
- Alcohol and body temperature
- Alcohol and the skin
- Alcohol, appetite and digestion
- Neurological effects of alcohol
- Alcohol, hormones and neurotransmitters
- Alcohol and pain
- Alcohol, blood pressure, heart disease and stroke
- Women, pregnancy, children and alcohol
- Alcohol tolerance
- Alcohol, blood glucose and diabetes
- Alcohol intolerance, allergy and headache
- Alcohol and psychological disorders
- Alcohol and vitamin, mineral and protein deficiency
- Alcohol-drug interactions

2 Responses to "Iron"