- Calcium facts: functions, supplements effects Linus Pauling Institute
- Dietary Reference Intakes Institute Of Medicine
- List of foods containing calcium US Department of Agriculture
- Mineral waters calcium and magnesium content PubMed Central
- Tap water calcium content PubMed Central
- Calcium function, sources, hypocalcemia, hypercalcemia, supplements Office of Dietary Supplements
- Calcium blood test Labtestsonline
- Nutrient deficiencies after bariatric surgery Endojournals
- Small intestinal bacterial overgrowth and hypocalcemia Emedicine
- Hypocalcemia Emedicine
- Hypercalcemia Emedicine
- Milk-alkali syndrome definition Emedicine
- WDHA syndrome Emedicine
- A systemic review of elevated blood pressure and consumption of dairy foods Journal of Human Hypertension
- Calcium intake and health maintenance Foodandnutritionresearch.net
- Calcium supplements benefits, side effects Natural Medicines Comprehensive Database
- Calcium supplements pregnancy categories Drugs.com
- Calcium and vitamin D in treatment of osteoporosis PubMed Central
- Oxalate and calcium absorption The American Journal of Clinical Nutrition
- Phytates and calcium absorption Arizona Cooperative Extension
- Calcium decreases the absorption of heme ad nonheme iron The American Journal of Clinical Nutrition
- Caffeine and osteoporosis Drugs.com
- Alcohol and osteoporosis National Institute of Alcohol Abuse and Alcoholism
- The effects of caffeine on bone PubMed
- Vitamin D and calcium supplementation to prevent fractures The U.S. Preventive Services Task Force
- Effects of calcium phosphate supplements on blood phosphate and calcium levels Nutrition Journal
- Calcium and vitamin D3 supplements in elderly Annals of Internal Medicine
- Diuretics and calcium homeostasis UpToDate
- Calcium supplements benefits and risks Medscape
- Effect of a combination of calcium and vitamin D supplements on kidney stones PubMed
- Calcium and vitamin D supplements to prevent osteoporosis during corticosteroid therapy PubMed
- Vegan supplements The Vegetarian Resource Group
- Calcium and vitamin D deficiency and risk of rickets The American Journal of Clinical Nutrition
- The health benefits of calcium citrate malate PubMed
- Strategies for prevention of calcium oxalate stones PubMed Central
- Lifestyle and sociodemographic factors as determinants of blood lead levels in elderly women PubMed
- Dietary factors [calcium phosphate or dicalcium phosphate dihydrate] in the prevention of dental caries PubMed
- Long-term remineralizing effect of casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) on early caries lesions in vivo PubMed
- Coral calcium carbonate absorption PubMed
- Calcium gluconate and chloride in hyperkalemia PubMed Central
- Bio-calcium from pearl shells PubMed
- Blackstrap molasses Indobase.com
- Vitamin D and fractures due to osteoporosis in elderly Cochrane
- Dietary intervention in idiopathic hypercalciuria Cochrane
- Calcium, magnesium and potassium supplements effect on primary hypertension Cochrane
- Calcium and stroke Cochrane
- Calcium supplementation and incident kidney stone risk PubMed
- Calcium supplements and risk of kidney stones in treatment of osteoporosis PubMed
- Calcium supplements and high blood pressure PubMed
- Calcium Intakes and Prostate Cancer Risk Journal of The National Cancer Institute
- EU approved food additives with E-numbers Food Standards Agency
- Calcium metabolism in health and disease Clinical Journal of the American Society of Nephrology
- Calcium deposits in soft tissues Harvard.edu
- Elemental calcium GlobalRPh
- Calcium chloride vs gluconate for injection Institute for Safe Medication Practices
- Moon HS et al, Hypocalcemia and hypokalemia due to hyperventilation syndrome in spinal anesthesia -A case report PubMed Central
- Treatment of hypomagnesemia with hypocalcemia Emedicine
- Calcium/magnesium intake ratio PubMed Central
- Calcium intake and risk of cardiovascular disease PubMed
- Calcium absorption from kale The American Journal of Clinical Nutrition
- Health effects of hard water PubMed Central
- Hardness in drinking water World Health Organization
- Soybean phytate content: the effect on calcium absorption The American Journal of Clinical Nutrition
- Calcium loss in sweat PubMed
- Calcium US Department of Agriculture
- Protein intake, calcium balance and health consequences European Journal of Clinical Nutrition
- Diet, fluid and supplements for prevention of nephrolithiasis PubMed Central
- Recurrent nephrolithiasis in adults: comparative effectiveness of preventive medical strategies Agency for Health Research and Quality
- Hypocalcemia – infants MedlinePlus
Calcium
What is calcium and what are its functions?
Calcium is an essential mineral. It gives strength to the bones and teeth and enables proper functioning of the nerves, muscles, gut, heart and blood vessels. It also participates in blood coagulation and production of energy from carbohydrates [1].
The chemical symbol for calcium is Ca.
How much calcium do you need?
The Recommended Dietary Allowance (RDA) for calcium for adults has been set at 1,000 mg (1 g) per day [1]. The average calcium intake in Americans (data from 2003-2006) is about 700-1,200 mg/day and is lower in women than in men [6].
Chart 1. Recommended Dietary Allowance (RDA) for calcium |
|
| AGE | RDA (mg/day) |
| Infants 0-6 months | 200 (Adequate Intake)* |
| Infants 7-12 months | 260 (Adequate Intake) |
| Children 1-3 years | 700 |
| Children 4-8 years | 1,000 |
| 9-18 years, including pregnant and breastfeeding women | 1,300 |
| Adults 19-70 years, including pregnant and breastfeeding women | 1,000 |
| Adults 71+ years | 1,200 |
Chart 1. source: The Food and Nutrition Board of the U.S. Institute of Medicine (IOM) [1] *Breast milk of healthy mothers should provide enough calcium for exclusively breastfed infants 0-6 months of age [1,3].
Foods Rich in Calcium
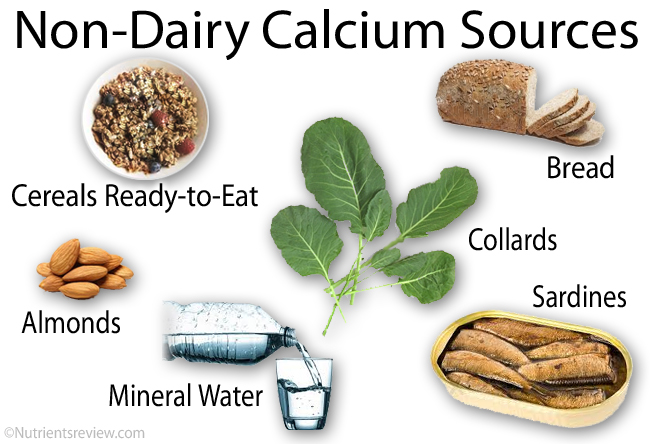
Common foods rich in calcium include dairy products, calcium-fortified foods, fish with edible bones, almond milk, radishes and certain mineral waters.
Picture 1. Non-dairy foods high in calcium
Chart 2. List of foods high in calcium |
|
DAIRY |
CALCIUM (mg) |
| Cheese, American pasteurized | 700-1,000 |
| Cheese, Gruyere, romano, Swiss (2.5 oz, 70 g) | 700-750 |
| Cheese, blue, brick, caraway, cheddar, colby, edam, gouda, gout, Mexican blend, monterey, muenster, provolone, Roquefort, Swiss-processed, tilsit (2.5 oz, 70 g) | 400-600 |
| Milk, sheep (1 cup, 237 mL) | 470 |
| Yogurt, plain (6 oz, 170 g) | 350 |
| Mozzarella (2.5 oz, 70 g) | 350-670 |
| Cheese, feta (2.5 oz, 70 g) | 350 |
| Milk cow/goat, nonfat, skim, whole (1 cup, 237 mL) | 300 |
| Cheese, brie, camembert, Ricotta (2.5 oz, 70 g) | 150-300 |
| Whey, sweet, powder (1 oz, 28 g) | 220 |
| Cheese, cottage, cream, neufchatel (2.5 oz, 70 g) | 60 |
NON-DAIRY |
CALCIUM (mg) |
Meat, Fish |
|
| Sardines, Atlantic, with bones (1 can, 92 g) | 350 |
| Canned mackerel and salmon (pink, chum, sockeye) with bones (1 can, 92 g) | 200-250 |
| Crabs, cuttlefish, shrimps, canned (3 oz, 85 g) | 100-150 |
| Carp, burbot, herring, trout (3 oz, 85 g) | 50-80 |
Cereals |
|
| Granola bar (60 g) | 200 |
| Bread, wheat, white or whole-grain (2 small slices, 60 g) | 40-80 |
Vegetables, Beans |
|
| Radishes, oriental, dried (1/2 cup, 60 g) | 360 |
| Lambsquarters (1/2 cup, 90 g) | 230 |
| Taro (1 cup, 137 g) | 200 |
| Blackstrap molasses (1 tbsp, 20 g) [42] | 170 |
| Amaranth leaves, collards, turnip greens (1/2 cup, ~80 g) | 120-135 |
| Soybeans, green, boiled (1/2 cup, 90 g) | 130 |
| Cowpeas (1/2 cup, 100 g) | 100 |
| Tempeh (1/2 cup, 80 g) | 90 |
| Chinese cabbage, bok choi; kale, Scotch; okra (1/2 cup, ~80 g) | 70-85 |
| Carrots, boiled (1/2 cup, 75 g) | 50 |
Nuts, Seeds |
|
| Almond milk (1 cup, 237 mL) | 450 |
| Chia seeds (1 oz, 28 g) | 180 |
| Chestnuts, Japanese, dried (1 cup, 150 g) | 110 |
| Sesame seeds (1 tbsp, 9 g) | 90 |
| Almonds (1 oz, 28 g) | 80 |
| Coconut water (1 cup, 237 mL) | 60 |
Fruits |
|
| Figs, dried (1/2 cup, 75 g) | 120 |
| Kiwi fruit, orange, prickly pear (1 fruit or 1 cup) | 70 |
| Prunes (1/2 cup, 60 g) | 50 |
Water |
|
| Mineral water (1 cup, 237 mL) [4] | 0-130 |
| Tap water (1 cup, 137 mL) [5] | 0-35 |
EXAMPLES OF CALCIUM-FORTIFIED FOODS AND JUICES |
CALCIUM (mg) |
| Cereals, ready-to-eat (1 cup, prepared with water) | 100-1,000 |
| Tofu with calcium sulfate (1 block, 80 g) | 550 |
| Formulated bar (55 g) | 530 |
| Milk (1 cup, 237 mL) | 500 |
| Cornmeal, self-rising (1 cup, 237 mL) | 500 |
| Bread, wheat, white, fortified (2 small slices, 60 g) | 400 |
| Orange juice (1 cup, 237 mL) | 350 |
| Fruit or vegetable juice, soy milk, rice drink (1 cup, 237 mL) | 200-350 |
| Cocoa powder (1 packet, 15 g) | 200 |
| English muffin with calcium propionate (57 g) | 100 |
Chart 2. source: US Department of Agriculture (USDA.gov) [3]
What is calcium from foods good for?
Osteoporosis
Adequate calcium intake along with physical activity throughout life may reduce the risk of osteoporosis at old age [6]. The bone mineral density (BMD) increases until about 30 years of age and then starts to decline slowly. The higher the calcium intake until 30, the higher the peak bone density after 30 [6].
Kidney Stones
In 2 systematic reviews (2009, 2013), researchers have found only a weak association between high calcium intake and reduced risk of kidney stones [67,68].
Some studies suggest calcium supplements in doses greater than 1,000 mg/day, especially when taken with vitamin D, but not calcium from food, can increase the risk of kidney stones [6,30]. In two systematic reviews from y. 2008 and 2012, researchers have found no association between calcium supplements and kidney stones, though [47,48].
High Blood Pressure
In the 1996 DASH feeding study, high calcium diet including fruits and dairy (~1,200 mg Ca/day) for 8 weeks resulted in a decrease of the upper (systolic) blood pressure in individuals with high blood pressure by up to 11.5 mm Hg more than a control diet low in fruits and dairy (~400 mg Ca/day) [1].
In one 2012 systematic review of studies, high intake of low-fat dairy was associated with 16% decrease, and high intake of cheese (high-fat dairy) with no significant decrease of high blood pressure [14].
From these studies, it is still not clear, was it calcium or some other food ingredient that was associated with decreased blood pressure.
Tooth Decay
In one 1994 study in 65-87 years old women, higher calcium intake was associated with less dental caries [36].
Health Effects of Hard Water
Hard water contains high amounts of calcium and/or magnesium. For some individuals, especially vegans, who may get little calcium from food, hard water can be a convenient source of calcium. Bottled mineral waters are usually harder than tap water and this is usually harder than most bottled “plain” waters.
According to World Health Organization (WHO), water hardness has neither beneficial or harmful effects on health [62].
Can consuming too much calcium be bad for you?
The Institute of Medicine in the U.S. has set the Tolerable Upper Intake Level (UL) for calcium–the intake (from foods and supplements) unlikely to cause adverse effects in most healthy individuals 1 year or more of age–at 2,000-3,000 mg/day [1].
Men: Prostate Cancer
In several, but not all studies, high calcium intake (>1,000 mg/day) from either foods or supplements, and high dairy intake were associated with increased risk of prostate cancer [1,50]. Until more is known, Linus Pauling Institute in the U.S. recommends men to limit calcium intake to 1,000-1,2000 mg/day [1].
In one 2013 systematic review, researchers have found no convincing association between high calcium intake and other types of cancer (breast, lung, colorectal, endometrial) [15].
Coronary Heart Disease and Heart Attack
Results of studies of calcium intake on heart disease are controversial. In one study in women, high calcium intake (>1,400 mg/day) was associated with increased and in another study with decreased mortality due to heart disease [6], but one 2012 review of studies has found no association between calcium intake and coronary heart disease [59].
A Low-Calcium Diet
If you have a chronic kidney disease and tend to have elevated blood calcium levels, your doctor may recommend you to decrease calcium intake by eating more low-calcium foods and limit, but not necessary completely avoid, calcium-rich foods.
Low-calcium diet is NOT recommended to individuals with increased risk of calcium kidney stones [44,47].
Chart 4. Low-Calcium and Calcium-Free Foods |
|
| FOOD | CALCIUM (mg) |
| Kale, squash, winter (1/2 cup, 65 g) | 45 |
| Legumes: beans, lentils, peas (1/2 cup) | 20-35 |
| Broccoli (1/2 cup, 40 g) | 30 |
| Nuts: hazelnuts, macadamia, peanuts, pistachios, walnuts (1 oz, 28 g) | 20-30 |
| Meats: beef, chicken, lamb, pork, turkey, veal (3 oz, 85 g) | 10-30 |
| Fruits: apple, apricot, banana, blackberries, currants, cherries, elderberries, grapes, mango, peach, pear, pineapple, raspberries, strawberries (1 serving = berries: 1/2 cup, other: 1 cup or 1 fruit) | 10-30 |
| Potato, sweet potato, yam (1 cup, 160 g) | 10-30 |
| Sunflower seeds (1 oz, 28 g) | 25 |
| Egg (50 g) | 25 |
| Rice, white or brown, regular or parboiled; pasta: macaroni, spaghetti (1 cup, 150 g) | 20 |
| Tilefish, mackerel without bones (3 oz, 85 g), oyster, tuna (1 can, 92 g) | 5-20 |
| Bulgur, buckwheat, couscous, millet (1 cup, 170 g) | 5-20 |
| Tomato (150 g), lettuce (1 cup), lemon (60 g), raisins (1 oz, 28 g) | 15 |
| Butter, coconut meat, honey, jam, margarine, oils, table sugar, vinegar (1 tbsp, 15-20 g), cornmeal, cornflakes, popcorn, distilled alcohol beverages, sausages, tea (ice, green, herbal, black) (1 serving) | 0-5 |
Chart 4. source: US Department of Agriculture (USDA.gov) [3]
Calcium Absorption and Excretion
Most of calcium is absorbed in the small intestine [6,65]. Oxalic acid (oxalate) found in spinach and rhubarb, and phytic acid (phytate) in dried beans and wheat bran inhibit calcium absorption, so these foods are not good sources of calcium [1]. Calcium from kale [60] and soybeans [63] is absorbed well. Most of calcium absorbed in excess of body needs is excreted with the urine [65]. Only small amounts of calcium are lost with sweat [64].
Normal Blood Calcium Levels Range
Normal blood calcium level range for adults is 8.6-10.2 mg/dL or 2.15-2.55 mmol/L [7].
Calcium Deficiency and Low Blood Calcium Levels (Hypocalcemia)
Calcium deficiency refers to low calcium stores in the body and may or may not lead to low blood calcium levels (hypocalcemia). About 1,000 grams (1 kg) of calcium is stored in the adult body, mainly in bones [52]. When you consume little or no calcium, calcium is resorbed from the bones into the blood, so the blood calcium levels do not fall, but in long-term calcium deficiency, the bones can become porous (osteoporosis).
Who is at risk to develop calcium deficiency?
- Women after menopause who have low estrogen levels are at increased risk of osteoporosis.
- Female athletes with anorexia nervosa and absent menstruation (amenorrhea) who have low estrogen levels are at increased risk of osteoporosis.
- Vegans
- Young alcoholics. Alcohol abuse in adolescence and young adulthood can affect calcium metabolism and increase the risk of osteoporosis later in life [6,23].
Hypocalcemia means blood calcium levels lower than 8.6 mg/dL. A short-term low dietary calcium intake (days/weeks) does not likely result in low blood calcium levels in healthy people.
What can cause calcium deficiency or low blood calcium levels?
- Hyperventilation, for example, due to anxiety or strenuous exercise, can result in transient hypocalcemia that is not detected by a blood test when you are not hyperventilating [56].
- A disorder of the parathyroid glands resulting in parathormone deficiency (hypoparathyroidism)
- Vitamin D deficiency
- Acute pancreatitis, acute kidney failure
- Celiac and Crohn’s disease, surgical removal of the stomach (gastric bypass, bariatric surgery) [8], small intestinal bacterial overgrowth (SIBO)
- Chronic alcoholism and anorexia nervosa
- Spread of the cancer to the bones
- Very low blood magnesium level (hypomagnesemia)
- Thyroid disease
- Surgical removal of overactive parathyroid glands
- Medications: amphotericin B, cinacalcet, cisplatin, enemas (sodium phosphate), estrogens, fluoride, foscarnet, gentamicin, phenobarbital, steroids, zoledronic acid, laxatives abuse (mineral oil, senna), long-term use of gastric acid-lowering drugs (cimetidine, omeprazole, aluminium and magnesium antacids) reduce calcium absorption [1,6].
Symptoms
- ACUTE: numbness and tingling in the fingers, toes and around the mouth (paresthesia), lightheadedness, excessive bleeding, stiffness and cramps in the legs (calves), spasms in the feet changed voice, muscle twitching [69], constipation, seizures, abnormal heart rhythm (arrhythmia) or even death
- CHRONIC: dry and itchy skin
Signs
- In chronic hypocalcemia: dry skin and hair, psoriasis, brittle nails, cataracts, memory loss (dementia)
Treatment of hypocalcemia includes calcium supplements and treatment of the underlying disorders.
Rickets and Osteoporosis
- In children, long-term calcium deficiency with or without vitamin D deficiency can result in poor calcium mineralization of bones ─ soft bones or rickets.
- In adults, calcium deficiency can result in low bone density ─ osteoporosis.
- References: [33]
Dental Fluorosis
Low dietary calcium and high fluoride intake, mainly by drinking water high in fluoride, can result in teeth discoloration (dental fluorosis).
Sources: Emedicine [9,10]
Calcium Supplements
Types of Oral Calcium Supplements Without Prescription (Over-The-Counter)
- Calcium carbonate can be used as a calcium supplement or antacid.
- “Coral calcium” or “marine calcium” supplements are derived from coral reefs and contain calcium carbonate and magnesium. In one small study in Japan, coral calcium carbonate was better absorbed than regular calcium carbonate [39], but there is no scientific evidence about its superiority over other calcium supplements.
- “Bio-calcium” obtained from pearl shells contains calcium carbonate, which is, according to few studies, no more effective than calcium carbonate from other sources [41].
- “Rock calcium” is a general term for inorganic calcium derived from limestone. Calcium carbonate and citrate are examples of rock calcium.
- Calcium citrate and citrate malate are appropriate for individuals with low gastric acid and increased risk of kidney stones.
- Calcium magnesium citrate is a calcium and magnesium supplement.
- Calcium lactate and gluconate are highly soluble but bulky, so they are mostly used as powders for solutions.
- Calcium phosphate is usually available in combination with vitamin D3.
- Calcium oxide (“lime”) and hydroxide (“slaked lime”) are sometimes used in multivitamin/mineral supplements and rarely, for example in Japan, as individual supplements, which are produced from oyster shells. They are more alkaline than other calcium supplements.
- In calcium orotate, calcium is combined with orothic acid, in calcium D-glucarate with glucaric acid, in calcium osporotate with aspartic, orothic and citric acid, in calcium amino acid chelates with hydrolyzed vegetable protein and in calcium AEP with amino ethanol phosphate. These supplements are often advertised to have greater bioavailability, but they have not been proven to be more effective than other calcium supplements.
- Calcium hydroxiapatite is derived from bovine bones.
- References: [6]
Available oral forms: tablets, capsules, chews, powder and liquids.
Chart 5. Calcium carbonate vs calcium citrate |
||
| PROPERTIES | CALCIUM CARBONATE | CALCIUM CITRATE |
| Uses | Calcium supplement, antacid (tums) | Calcium supplement |
| Amount of elemental calcium | 40% (500 mg calcium carbonate contains 200 mg Ca) | 21% (500 mg calcium citrate contains 105 mg Ca) |
| Recommended intake | With foods | With or without foods |
| Absorption in low gastric acid (achlorhydria, hypochlorhydria) | Poor | Good |
| Short-term side effects | Constipation, bloating | Less side effects than calcium carbonate |
| Risk of kidney stones with long-term use | Possibly | No |
Chart 5. sources: [6,34,35]
Calcium Injections
In severe hypocalcemia, your doctor can give you an injection of calcium gluconate or chloride into a vein. These two supplements can be also used as antidotes to prevent adverse effects of hyperkalemia on the heart muscle but not to treat hyperkalemia itself [40].
Dosage
To treat calcium deficiency, a typical dose is 1 gram (1,000 mg) of elemental calcium per day [6]. It is your doctor who can prescribe the dose appropriate for you.
To know how much calcium you get from supplements you should check milligrams of elemental calcium, not milligrams of the the whole calcium compound.
Chart 6. Elemental Calcium |
|
| CALCIUM SUPPLEMENT | ELEMENTAL CALCIUM (mg of calcium in a 500 mg pill) |
| Ca oxide | 71% (355 mg) |
| Ca hydroxide | 54% (270 mg) |
| Ca carbonate | 40% (200 mg) |
| Ca phosphate, tribasic | 38% (190 mg) |
| Ca chloride | 27.2% (136 mg) |
| Ca acetate | 25.3% (126.5 mg) |
| Ca phosphate, dibasic | 23% (115 mg) |
| Ca citrate | 21% (105 mg) |
| Microcrystalline hydroxyapatite (MH) | 20% (100 mg) |
| Calcium chelates: orotate, aspartate | (about 100 mg) |
| Ca lactate | 13% (65 mg) |
| Ca gluconate | 9.3% (46.5 mg) |
| Ca gluceptate | 8.2% (41 mg) |
| Ca glubionate | 6.5% (32.5 mg) |
Chart 6. source: Globalrph.com (54), producers
Absorption and Bioavailability of Supplemental Calcium
Calcium is optimally absorbed when taken in doses up to 500 mg elemental calcium at once [6]. You can divide larger doses in half for better absorption.
Different calcium supplements are probably absorbed equally well and have about the same bioavailability. Unlike other supplements, calcium citrate and calcium citrate malate are absorbed well on an empty stomach and in low gastric acid (achlorhydria, hypochlorhydria) [6]. Calcium phosphate is less well absorbed, because phosphate binds to calcium in the gut and inhibits its absorption [26].
Possible Calcium Supplements Benefits
Calcium supplements are EFFECTIVE for:
- Prevention and treatment of calcium deficiency
- Preventing irregular heart rhythm in hyperkalemia (intravenous injection) [40]
- Lowering high phosphate levels in kidney failure
- Reducing gastroesophageal reflux and heartburn (calcium carbonate)
Calcium supplements are LIKELY EFFECTIVE for reducing thyroid hormone levels in people with a kidney failure
Calcium supplements MAY BE EFFECTIVE (low evidence or only slight effect):
- When taking along with vitamin D:
- For prevention of bone fractures in men after 65 and women after menopause with osteoporosis [18,43], and for prevention of bone loss in individuals who take steroids [31].
- For prevention of fluoride poisoning in children.
- When taking along with a low-fat or low-calorie diet: for reducing blood cholesterol levels.
Other sources: Linus Pauling Institute [1], Natural Medicines Comprehensive Database [16]
There is INSUFFICIENT EVIDENCE about calcium supplements effectiveness for preventing colorectal, prostate or other cancer, dental caries (tooth decay) [37,38], heart disease, high blood pressure [49], high blood pressure in pregnancy (pre-eclampsia), Lyme disease, metabolic syndrome, osteoporosis (in individuals who do not already have osteoporosis) [25], pregnancy-related leg cramps, diabetes, premenstrual syndrome (PMS), seizures, stroke or for promoting weight loss. Other references: [16,45,46].
Calcium supplements are POSSIBLY INEFFECTIVE for preventing breast cancer in postmenopausal women [16].
Calcium Supplements Safety: Side Effects, Toxicity
The Upper Tolerable Intake Limit (UL) for calcium–the intake unlikely to cause side effects in most healthy people–is: for 0-6 months: 1,000 mg/day; for 7-12 months: 1,500 mg/day; for 1-8 years: 2,500 mg/day; for 9-18 years: 3,000 mg/day; for 19-50 years: 2,500 mg/day and for 51 years and older: 2,000 mg/day [1].
Side effects of calcium supplements include constipation and bloating [6]. Injection of calcium chloride can irritate the veins or muscles [55].
Certain calcium supplements derived from bone meal, dolomite or oyster shells contain small amounts of lead, but calcium inhibits lead absorption in the gut, so the actual harm of lead is probably lower than the benefit from calcium supplements [1,29].
During Pregnancy
According to the U.S. Food and Drug Administration (FDA), pregnancy categories for calcium supplements are:
- “Not classified” for calcium carbonate, glubionate, phosphate
- Category C, which means harmful effects for the babies have been not proven but can not be excluded due to lack of human trials: calcium acetate, citrate, chloride, gluconate, lactate
- Source: Drugs.com: 17
High Blood Calcium Levels (Hypercalcemia)
Hypercalcemia means blood calcium higher than 10.5 mg/dL. High calcium intake from foods, water or supplements does not likely cause hypercalcemia in healthy individuals.
What can cause high blood calcium levels?
- Increased blood parathormone (PTH) level (hyperparathyroidism) due to a parathyroid tumor (adenoma) or other parathyroid gland disorder
- Cancer, especially bone metastases, and rare tumors called VIPomas
- Conditions that increase bone resorption or intestinal calcium absorption: prolonged immobilization, Paget’s disease, multiple myeloma, sarcoidosis, tuberculosis, systemic fungal infection, AIDS, advanced liver disease
- Kidney failure combined with high doses of calcium supplements (>2 g elemental Ca/day) or consumption of large amounts of milk, which can result in milk-alkali syndrome. If not recognized, milk-alkali syndrome may lead to kidney calcification and failure or even death.
- Vitamin D in doses exceeding 50,000 IU/day, calcium exceeding 2 g calcium/day, high doses of vitamin A, lithium, theophylline, thiazide diuretics (chlorothiazide), calcipotriene (calcipotriol), parathormone (PTH), calcium-based phosphate binders, estrogens
Symptoms: nausea, constipation, depression, weakness, muscle or joint aches, frequent urination, headache and, in severe cases, coma or death.
Treatment may include rehydration, diuretics and treatment of the cause.
Calcium Deposits
Calcium deposits, calcification or calcinosis means buildup of calcium or calcium-phosphate crystals in the body organs and their damage. Diet high in calcium does not likely cause calcium deposits [53]. Main causes include cancer, chronic hypercalcemia and hyperphosphatemia, especially in chronic kidney failure, high doses of calcium supplements (>2 g elemental Ca/day), sarcoidosis, tuberculosis, scleroderma and genetic or autoimmune processes.
Sources: Emedicine: [11,12,13]
Calcium-Nutrients Interactions
- Oxalate in spinach, rhubarb, beet greens, Swiss chard and beans can decrease calcium absorption from these foods, but not likely from other foods [6,19]. On the other hand, calcium reduces absorption of oxalate thus possibly reducing the risk of calcium-oxalate kidney stones.
- Phytates in seeds, nuts and wheat bran can decrease calcium absorption from these and other foods [20].
Frequently Asked Questions
1. Do vegans need to take calcium supplements?
Not necessary. Bread and calcium-enriched foods are good sources of calcium.
2. Which calcium supplements are vegan?
Most calcium supplements are vegan. Calcium lactate (E327) is usually derived from non-animal sources and only occasionally from whey, so it is “typically vegan.” Non-vegan supplements are calcium caseinate, stearate and hydroxyapatite, and supplements derived from bone meal, bone flour and shellfish shells [32].
3. Does caffeine causes calcium deficiency?
Caffeine slightly decreases calcium absorption but it is not clear if this has any importance for health [6,16,22,24].
Minerals
- Fructose
- Galactose
- Glucose
- Isomaltose
- Isomaltulose
- Lactose
- Maltose
- Mannose
- Sucrose
- Tagatose
- Trehalose
- Trehalulose
- Xylose
- Erythritol
- Glycerol
- Hydrogenated starch hydrolysates (HSH)
- Inositol
- Isomalt
- Lactitol
- Maltitol
- Mannitol
- Sorbitol
- Xylitol
- Fructo-oligosaccharides (FOS)
- Galacto-oligosaccharides (GOS)
- Human milk oligosaccharides (HMO)
- Isomalto-oligosaccharides (IMO)
- Maltotriose
- Mannan oligosaccharides (MOS)
- Raffinose, stachyose, verbascose
- SOLUBLE FIBER:
- Acacia (arabic) gum
- Agar-agar
- Algin-alginate
- Arabynoxylan
- Beta-glucan
- Beta mannan
- Carageenan gum
- Carob or locust bean gum
- Fenugreek gum
- Galactomannans
- Gellan gum
- Glucomannan or konjac gum
- Guar gum
- Hemicellulose
- Inulin
- Karaya gum
- Pectin
- Polydextrose
- Psyllium husk mucilage
- Resistant starches
- Tara gum
- Tragacanth gum
- Xanthan gum
- INSOLUBLE FIBER:
- Cellulose
- Chitin and chitosan
- FATTY ACIDS
- Saturated
- Monounsaturated
- Polyunsaturated
- Short-chain fatty acids (SCFAs)
- Medium-chain fatty acids (MCFAs)
- Long-chain fatty acids (LCFAs)
- Very long-chain fatty acids (VLCFAs)
- Monoglycerides
- Diglycerides
- Triglycerides
- Vitamin A - Retinol and retinal
- Vitamin B1 - Thiamine
- Vitamin B2 - Riboflavin
- Vitamin B3 - Niacin
- Vitamin B5 - Pantothenic acid
- Vitamin B6 - Pyridoxine
- Vitamin B7 - Biotin
- Vitamin B9 - Folic acid
- Vitamin B12 - Cobalamin
- Choline
- Vitamin C - Ascorbic acid
- Vitamin D - Ergocalciferol and cholecalciferol
- Vitamin E - Tocopherol
- Vitamin K - Phylloquinone
- Curcumin
- FLAVONOIDS:
- Anthocyanidins
- Flavanols: Proanthocyanidins
- Flavanones: Hesperidin
- Flavonols: Quercetin
- Flavones: Diosmin, Luteolin
- Isoflavones: daidzein, genistein
- Caffeic acid
- Chlorogenic acid
- Lignans
- Resveratrol
- Tannins
- Tannic acid
- Alcohol chemical and physical properties
- Alcoholic beverages types (beer, wine, spirits)
- Denatured alcohol
- Alcohol absorption, metabolism, elimination
- Alcohol and body temperature
- Alcohol and the skin
- Alcohol, appetite and digestion
- Neurological effects of alcohol
- Alcohol, hormones and neurotransmitters
- Alcohol and pain
- Alcohol, blood pressure, heart disease and stroke
- Women, pregnancy, children and alcohol
- Alcohol tolerance
- Alcohol, blood glucose and diabetes
- Alcohol intolerance, allergy and headache
- Alcohol and psychological disorders
- Alcohol and vitamin, mineral and protein deficiency
- Alcohol-drug interactions

3 Responses to "Calcium"